What is a Podiatrist?
A podiatrist is a Doctor of Podiatric Medicine who treats the foot, ankle, and related structures of the leg. If you are having any pain, injuries, or abnormalities in these areas, it is best that you seek help from a podiatrist.
Podiatrists complete four years of training in a podiatric medical school. Their training is like that of other physicians, and they may go on to complete a fellowship training after a residency training. Some podiatrists are board certified meaning they have advanced training, clinical experience, and have taken an exam to prove their skills. Certifying boards for podiatry are the American Board of Foot and Ankle Surgery and the American Board of Podiatric Medicine. Podiatrists may work in private practices, hospitals, clinics, or they may even become professors at colleges of podiatric medicine.
While in college, those who want to be podiatrists often take biology, chemistry, and physics classes in preparation for podiatry school. In podiatry school, students study how the bones, nerves, and muscles work together to help you move around. Additionally, they study injuries and how to properly diagnose and treat them. Admittance into podiatric medical school requires the completion of 90 semester hours of undergraduate study with a good grade point average, and acceptable scores on the MCAT (Medical College Admission Test)
Podiatrists treat many different conditions such as: aching feet, ankle pain, bunions, corns, hammertoes, fungus, ingrown toenails, plantar fasciitis, sprains and more. Common forms of treatment for these conditions are physical therapy, drugs, or surgery. Podiatrists may also recommend corrective shoe inserts, custom-made shoes, plaster casts, and strappings to correct deformities.
Even if you are someone whose feet are in generally good condition, you should still visit a podiatrist to have your feet properly exfoliated and maintained, or to make sure you are looking after your feet properly.
Symptoms and Treatment of Morton’s Neuroma

Morton's neuroma is a painful foot condition that occurs when a nerve becomes compressed between the metatarsal bones, typically between the third and fourth toes. Patients may feel a sharp, burning, or stabbing pain in the ball of the foot, along with tingling, cramping, or numbness in the toes. It may feel as though a small object, such as a pebble, is stuck inside the shoe. As the condition progresses, the pain may become more frequent and intense. A podiatrist can diagnose Morton's neuroma through a physical exam and specific compression tests, sometimes supported by imaging. Treatment may involve custom shoe inserts to reduce pressure on the affected nerve or corticosteroid injections to reduce inflammation. If these measures do not relieve symptoms, surgery might be required to either remove the thickened nerve tissue or release the ligament causing the compression. If you experience symptoms of Morton's neuroma, it is suggested that you schedule an appointment with a podiatrist for appropriate treatment.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact James Tyler Vestile, DPM of Foot and Ankle Centers of Indiana. Our doctor will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our office located in Tipton, IN . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Morton's Neuroma
Morton's Neuroma, also called Intermetatarsal Neuroma or Plantar Neuroma, is a condition that affects the nerves of the feet, usually the area between the third and fourth toe. Neuroma refers to a benign growth that can occur in different parts of the body. Morton's Neuroma strictly affects the feet. This condition causes the tissue around the nerves that lead to the toes becoming thick, causing pain in the ball of the foot.
This condition can be caused by injury, pressure or irritation. Normally no lump will be felt, but instead burning pain in the ball of the foot will be experienced. Numbness and tingling may also occur. With the onset of this condition, a person may feel pain when tight or narrow shoes are worn. As the condition worsens, the pain may persist for days, or even weeks.
Persistent foot pain should always be a concern. The foot should be examined by a podiatrist if pain persists longer than a few days with no relief from changing shoes. The earlier the foot is examined and treated, the less chance there will be for surgical treatment.
There are some factors that can play a role in the development of Morton's Neuroma. These include wearing ill-fitting shoes that cause pressure to the toes, such as high heels. Also, high impact exercise may contribute to the cause of this condition. Morton’s Neuroma may also develop if the foot sustains an injury. Another cause includes walking abnormally due to bunions or flat feet. This causes excessive pressure and irritates the tissue. At times, people are affected for no determinable reason.
Podiatrists can alleviate the effects of this condition using a treatment plan to help decrease the pain and heal the foot tissue. Depending upon the severity of the Morton's Neuroma, the treatment plan can vary. For cases that are mild to moderate, treatments may include applying padding to the arch to relieve pressure from the nerve and reduce compression while walking. Ice packs can also help reduce swelling. The podiatrist may also create a custom orthotic device to support the foot and reduce compression and pressure on the affected nerve. The doctor will probably advise against partaking in activities that cause constant pressure on the affected area. They may provide wider shoes to ease the pressure from the toes. If these treatments do not relieve the symptoms of this condition, the doctor may use injection therapy.
Surgical treatment may be recommended by the podiatrist if all other treatments fail to provide relief. Normally, the podiatric surgeon will decide on either a surgical procedure that involves removal of the affected nerve or will choose surgery to release the nerve. After examination, the surgeon will decide on the best approach to treat the problem.
Recovery varies according to the type of surgical procedure. The patient will also be instructed on the best shoe wear to prevent the return of this condition, along with changes to workout routines, if this was a cause. Preventative measures are important in ensuring the condition does not return.
Managing Blisters on the Feet

Blisters are small fluid-filled pockets that form on the skin due to friction, heat, or irritation. On the feet, they are often caused by wearing tight shoes, prolonged walking or running, moisture buildup, or socks that rub against the skin. Common areas affected include the heels, toes, and soles. Symptoms of a blister include a raised, bubble-like area filled with clear fluid, often accompanied by redness, tenderness, or a burning sensation. Walking can become painful, and, if the blister breaks, it may become vulnerable to infection leading to increased redness, swelling, or pus. While many blisters heal on their own, recurring or infected blisters should be evaluated by a podiatrist. This type of doctor can treat and drain blisters safely, prevent infection, and recommend proper footwear or orthotics to stop future occurrences. They can also identify underlying issues like abnormal gait or foot structure. If you have a painful foot blister, it is suggested that you schedule an appointment with a podiatrist.
Blisters may appear as a single bubble or in a cluster. They can cause a lot of pain and may be filled with pus, blood, or watery serum. If your feet are hurting, contact James Tyler Vestile, DPM of Foot and Ankle Centers of Indiana. Our doctor can provide the care you need to keep you pain-free and on your feet.
Foot Blisters
Foot blisters are often the result of friction. This happens due to the constant rubbing from shoes, which can lead to pain.
What Are Foot Blisters?
A foot blister is a small fluid-filled pocket that forms on the upper-most layer of the skin. Blisters are filled with clear fluid and can lead to blood drainage or pus if the area becomes infected.
Symptoms
(Blister symptoms may vary depending on what is causing them)
- Bubble of skin filled with fluid
- Redness
- Moderate to severe pain
- Itching
Prevention & Treatment
In order to prevent blisters, you should be sure to wear comfortable shoes with socks that cushion your feet and absorb sweat. Breaking a blister open may increase your chances of developing an infection. However, if your blister breaks, you should wash the area with soap and water immediately and then apply a bandage to the affected area. If your blisters cause severe pain it is important that you call your podiatrist right away.
If you have any questions, please feel free to contact our office located in Tipton, IN . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Blisters
Blisters are pockets of fluid that occur under the top layer of your skin. These fluid pockets are usually filled with pus, blood, or serum. Blisters may itch or hurt and can appear as a single bubble or in clusters.
The most common types of blisters are friction blisters. This type of blister may be caused by wearing shoes that are too tight. Friction blisters can also occur on the hands. A change in temperature may also cause blisters on the feet. In the freezing air, frostbite on your toes can lead to blisters, as well as sunburn from hot weather.
The best way to treat a blister is to keep it clean and dry. Most blisters will get better on their own. Once the skin absorbs the fluid within the blister, it will flatten and eventually peel off. You should avoid popping your blister unless you podiatrist does it for you. Additional treatment options include applying an ice pack to the blister or using over-the-counter blister bandages to cover the affected area.
If your blister becomes discolored, inflamed, or worsens it is advised that you speak to your podiatrist. Blisters that are yellow, green, or purple may be infected and require immediate medical attention. Blisters that are abnormally colored may be a sign of a more serious underlying health condition such as herpes.
Why Toes Become Swollen or Discolored

Swollen or discolored toes can be alarming and uncomfortable, and they may point to a variety of underlying issues. These changes can result from something as simple as minor trauma, like stubbing a toe, or more serious problems such as infections, poor circulation, or inflammatory conditions. Blue or purple discoloration may indicate reduced blood flow or bruising, while redness and warmth could suggest an infection or gout. Swelling might also occur with arthritis or as a reaction to wearing ill-fitting shoes. In some cases, especially during colder months, conditions like chilblains or Raynaud’s phenomenon may cause color changes and discomfort. While some causes are temporary and harmless, others require prompt attention to avoid complications. If your toes are swollen, painful, or changing color without a clear reason, or if symptoms persist, it is suggested that you see a podiatrist to identify the cause and receive the right care.
Toe pain can disrupt your daily activities. If you have any concerns, contact James Tyler Vestile, DPM of Foot and Ankle Centers of Indiana. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Causes Toe Pain?
Most severe toe pain is caused due to a sports injury, trauma from dropping something heavy on the toe, or bumping into something rigid. Other problems can develop over time for various reasons.
Toe pain can be caused by one or more ailments. The most common include:
- Trauma
- Sports injury
- Wearing shoes that are too tight
- Arthritis
- Gout
- Corns and calluses
- Hammertoe
- Bunions
- Blisters
- Ingrown toenails
- Sprains
- Fractures (broken bones)
- Dislocations
When to See a Podiatrist
- Severe pain
- Persistent pain that lasts more than a week
- Signs of infection
- Continued swelling
- Pain that prevents walking
Diagnosis
In many cases the cause of toe pain is obvious, but in others, a podiatrist may want to use more advanced methods to determine the problem. These can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatments for toe pain and injuries vary and may include shoe inserts, padding, taping, medicines, injections, and in some cases, surgery. If you believe that you have broken a toe, please see a podiatrist as soon as possible.
If you have any questions please feel free to contact our office located in Tipton, IN . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Toe Pain
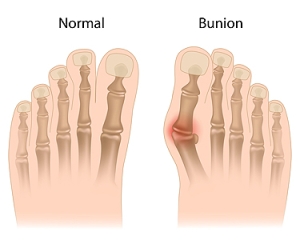
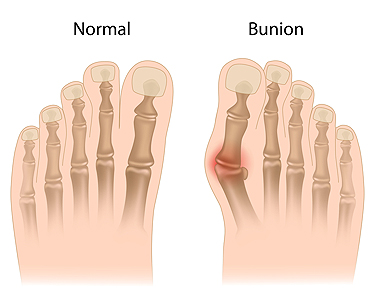
Toe pain can originate from corns, calluses, hammertoes, and bunions, as well as ingrown toenails, sprains, fractures, and dislocations. Corns develop as the toe rubs against the inside of a shoe which causes the skin to thicken as a form of protection. A corn is typically cone-shaped and has a small, hardened spot that points inward. When a corn is pressed into the skin, the toe becomes painful. Corns usually form on the top or side of the toe. A callus is also a thickened patch of skin that generally forms on the bottom of the foot. Calluses are the result of friction from the toe rubbing against the inside of a shoe. They may also occur by walking barefoot or having flat feet. A hammertoe is a bump on the knuckle of the second toe that is produced by wearing shoes that are too short for your feet. The bony protrusion rubs against the top of the shoe causing pain and irritation. A bunion is a malformation of the big toe. The base of the big toe pushes away from the smaller toes, forcing the top of the big toe to press toward the other toes. Bunions can be hereditary, or they can result from injury to the toe joint or from wearing high heels with a narrow toe box. The toe becomes inflamed, and a bump may develop at the end of the misplaced bone. Ingrown toenails typically affect the big toe and its surrounding skin. The nail will dig into the skin and become painful. Wearing tight or narrow shoes that compress the big toe causes the nail to grow into the fleshy part of the toe. Cutting toenails incorrectly can also add to the development of an ingrown toenail. A toe sprain originates from a torn or stretched ligament. Strapping the injured toe to the toe next to it for stabilization is common. A broken or fractured toe usually occurs from trauma like dropping a heavy object on it or bumping into something extremely hard and rigid. Osteoporosis, a thinning of the bones, can also bring about toe fractures.
Any of the conditions mentioned can lead to pain and irritation. While some are more serious than others, seeking an examination and diagnosis from a podiatrist is a good idea. A podiatrist can treat each ailment and get you back on your feet again without pain.
Simple Exercises That May Help Ease Bunion Discomfort
Bunions can cause pain, stiffness, and swelling near the big toe joint. While bunions do not go away on their own, gentle exercises may help reduce discomfort, improve flexibility, and slow their progression. One helpful move is the toe stretch where you simply pull the big toe gently into alignment and hold for several seconds. Another is the towel scrunch. This involves placing a towel flat on the floor and using your toes to scrunch it toward you, which can strengthen the foot muscles. Try toe spreading by placing small spacers or your fingers between your toes and holding for a short time. Additionally, rolling a ball under your foot can also ease tension. These exercises should be done daily and combined with supportive shoes and foot care. If you have bunion pain, it is suggested that you see a podiatrist for appropriate treatment.
If you are suffering from bunions, contact James Tyler Vestile, DPM of Foot and Ankle Centers of Indiana. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
A bunion is formed of swollen tissue or an enlargement of boney growth, usually located at the base joint of the toe that connects to the foot. The swelling occurs due to the bones in the big toe shifting inward, which impacts the other toes of the foot. This causes the area around the base of the big toe to become inflamed and painful.
Why Do Bunions Form?
Genetics – Susceptibility to bunions are often hereditary
Stress on the feet – Poorly fitted and uncomfortable footwear that places stress on feet, such as heels, can worsen existing bunions
How Are Bunions Diagnosed?
Doctors often perform two tests – blood tests and x-rays – when trying to diagnose bunions, especially in the early stages of development. Blood tests help determine if the foot pain is being caused by something else, such as arthritis, while x-rays provide a clear picture of your bone structure to your doctor.
How Are Bunions Treated?
- Refrain from wearing heels or similar shoes that cause discomfort
- Select wider shoes that can provide more comfort and reduce pain
- Anti-inflammatory and pain management drugs
- Orthotics or foot inserts
- Surgery
If you have any questions, please feel free to contact our office located in Tipton, IN . We offer the newest diagnostic and treatment technologies for all your foot care needs.
What Are Bunions?
Bunions are large bony bumps at the base of the big toe. Medically known as hallux valgus, a bunion is a misalignment of the metatarsophalangeal joint, or big toe joint. The misalignment will generally worsen with time if left untreated.
The exact cause of bunions is unknown, with genetics seen as a potential cause. High heels and poorly-fitted footwear, rheumatoid arthritis, and heredity all seem to be potential factors behind the exacerbation of bunions. Women have been found to be more likely to develop bunions in comparison to men.
Bunions do not always produce symptoms. The best way to tell is if the big toe is pushing up against the next toe and there is a large protrusion at the base of the big toe. You may or may not feel pain. Redness, swelling, and restricted movement of the big toe may be present as well.
Podiatrists use a variety of methods to diagnose bunions. If there are symptoms present, podiatrists will first consider that it is a bunion. If not, a physical examination will be conducted to check function of the big toe. Finally, an X-ray may be taken to view the extent of the bunion and confirm it is a bunion.
Typically, nonsurgical methods are used to treat bunions, unless the bunion has become too misaligned. Orthotics, icing and resting the foot, roomier and better fitted shoes, taping the foot, and pain medication are usually utilized first. If the bunion doesn’t go away or causes extreme pain, surgery may be required. Surgeons will either remove part of the swollen tissue or bone to straighten the toe out.
If you have a bunion, it is recommended to see a podiatrist. The longer it is left untreated, the worse it may get. Podiatrists can properly diagnose and treat a bunion before it gets worse.