Neuropathy
Neuropathy is a condition in which the nerves in the body become damaged from a number of different illnesses. Nerves from any part of the body, including the foot, can be damaged. There are several forms of neuropathy including peripheral neuropathy, cranial neuropathy, focal neuropathy, and autonomic neuropathy. Furthermore there is also mononeuropathy and polyneuropathy. Mononeuropathies affect one nerve while polyneuropathies affect several nerves. Causes of neuropathy include physical injury, diseases, cancers, infections, diabetes, toxic substances, and disorders. It is peripheral neuropathy that affects the feet.
The symptoms of neuropathy vary greatly and can be minor such as numbness, sensation loss, prickling, and tingling sensations. More painful symptoms include throbbing, burning, freezing, and sharp pains. The most severe symptoms can be muscle weakness/paralysis, problems with coordination, and falling.
Podiatrists rely upon a full medical history and a neurological examination to diagnose peripheral neuropathy in the foot. More tests that may be used include nerve function tests to test nerve damage, blood tests to detect diabetes or vitamin deficiencies. Imaging tests, such as CT or MRI scans, might be used to look for abnormalities, and finally nerve or skin biopsies could also be taken.
Treatment depends upon the causes of neuropathy. If the neuropathy was caused by vitamin deficiency, diabetes, infection, or toxic substances, addressing those conditions can lead to the nerve healing and sensation returning to the area. However if the nerve has died, then sensation may never come back to the area. Pain medication may be prescribed for less serious symptoms. Topical creams may also be tried to bring back sensation. Electrical nerve stimulation may be used for a period of time to stimulate nerves. Physical therapy can strengthen muscle and improve movement. Finally surgery might be necessary if pressure on the nerve is causing the neuropathy.
If you are experiencing sensation loss, numbness, tingling, or burning sensations in your feet, you may be experiencing neuropathy. Be sure to talk to a podiatrist to be diagnosed right away.
Treatment Options for Plantar Warts

Plantar warts develop on the bottom of the foot due to exposure to the human papillomavirus, or HPV, often found in warm, damp environments. Some plantar warts resolve on their own, but others may require treatment. It is important to seek professional care, as attempting to remove a plantar wart at home improperly can damage healthy skin and increase discomfort. A podiatrist can provide several options, including applying salicylic acid to break down the wart over time or using cryotherapy to freeze it off with liquid nitrogen. If the wart is persistent, additional treatments may be necessary. Among them are curettage to remove the wart surgically, laser therapy to target the blood vessels feeding the wart, or prescription medication applied directly to the affected area. Plantar warts that are deep or cause pain may require a combination of treatments for effective removal. If you notice an unusual or painful growth on the bottom of your foot, it may indicate a plantar wart, and it is suggested that you schedule an appointment with a podiatrist for an exam, diagnosis, and treatment options.
Plantar warts can be very uncomfortable. If you need your feet checked, contact James Tyler Vestile, DPM from Foot and Ankle Centers of Indiana. Our doctor will assist you with all of your foot and ankle needs.
About Plantar Warts
Plantar warts are the result of HPV, or human papillomavirus, getting into open wounds on the feet. They are mostly found on the heels or balls of the feet.
While plantar warts are generally harmless, those experiencing excessive pain or those suffering from diabetes or a compromised immune system require immediate medical care. Plantar warts are easily diagnosed, usually through scraping off a bit of rough skin or by getting a biopsy.
Symptoms
- Lesions on the bottom of your feet, usually rough and grainy
- Hard or thick callused spots
- Wart seeds, which are small clotted blood vessels that look like little black spots
- Pain, discomfort, or tenderness of your feet when walking or standing
Treatment
- Freezing
- Electric tool removal
- Laser Treatment
- Topical Creams (prescription only)
- Over-the-counter medications
To help prevent developing plantar warts, avoid walking barefoot over abrasive surfaces that can cause cuts or wounds for HPV to get into. Avoiding direct contact with other warts, as well as not picking or rubbing existing warts, can help prevent the further spread of plantar warts. However, if you think you have developed plantar warts, speak to your podiatrist. He or she can diagnose the warts on your feet and recommend the appropriate treatment options.
If you have any questions please feel free to contact our office located in Tipton, IN . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
All About Plantar Warts
Plantar warts are warts that are only found on the feet, hence the term “plantar”, which means “relating to the foot.” They are caused by the human papillomavirus, or HPV, and occur when this virus gets into open wounds on the feet. The warts themselves are hard bumps on the foot. They are easily recognizable, mostly found on the heels or ball of the foot. Plantar warts are non-malignant, but they can cause some pain, discomfort, and are often unsightly. Removing them is a common step toward treating them.
Plantar warts can cause some pain while standing, sometimes felt as tenderness on the sole of your foot. Unless the wart has grown into the foot behind a callus, you will be able to see the fleshy wart. A podiatrist should only be consulted if there is an excessive amount of pain. Plantar warts are not cancerous or dangerous, but they can affect your walking and continually reappear. Anyone who suffers from diabetes or a compromised immune system disease should seek out care immediately.
Podiatrists are easily able to diagnose plantar warts. They usually scrape off a tiny bit of the rough skin to make tiny blood clots visible and examine the inside of warts. However, a biopsy can be done if the doctor is not able to diagnose them from simply looking at them. Although plantar warts usually do not require an excessive amount of treatment, there are ways to go about removing them. A common method is to freeze them off using liquid nitrogen, removing them using an electrical tool, or burning them off via laser treatment. For a less invasive treatment option, topical creams can be used through a doctor’s prescription. This treatment method takes more time, however. Keep the wart covered for protection in between daily treatments.
The best way to avoid developing plantar warts is to avoid walking barefoot in public places. Avoid this especially if you have open sores or cuts on your feet. It is also important to avoid direct contact with warts in general, as they are highly contagious.
Reminder: When Was the Last Time...?
Types of Surgery for Ankle Arthritis

Ankle arthritis occurs when the smooth cartilage in the joint wears away, causing pain, swelling, and stiffness. If nonsurgical treatments no longer provide relief, ankle surgery may help to restore movement and reduce pain. Several procedures address different levels of joint damage. Ankle debridement and removal of extra bone growths and damaged tissue can improve mobility in mild cases. Ankle fusion, also called arthrodesis, permanently joins bones to stop painful friction, although it limits flexibility. Cartilage repair methods, such as microfracture or grafting, aim to regrow lost cartilage and preserve movement. In severe cases, ankle replacement, or arthroplasty, removes damaged joint surfaces and replaces them with artificial parts to restore function. This option helps to maintain flexibility but requires careful long-term management. A podiatrist can assess your symptoms, recommend the best procedure, and provide guidance for recovery. If you have ankle pain that interferes with daily activities, it is suggested that you schedule an appointment with a podiatrist for a diagnosis and appropriate treatment options.
Ankle pain can be caused by a number of problems and may be potentially serious. If you have ankle pain, consult with James Tyler Vestile, DPM from Foot and Ankle Centers of Indiana. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Ankle pain is any condition that causes pain in the ankle. Due to the fact that the ankle consists of tendons, muscles, bones, and ligaments, ankle pain can come from a number of different conditions.
Causes
The most common causes of ankle pain include:
- Types of arthritis (rheumatoid, osteoarthritis, and gout)
- Ankle sprains
- Broken ankles
- Achilles tendonitis
- Achilles tendon rupture
- Stress fractures
- Bursitis
- Tarsal tunnel syndrome
- Plantar fasciitis
Symptoms
Symptoms of ankle injury vary based upon the condition. Pain may include general pain and discomfort, swelling, aching, redness, bruising, burning or stabbing sensations, and/or loss of sensation.
Diagnosis
Due to the wide variety of potential causes of ankle pain, podiatrists will utilize a number of different methods to properly diagnose ankle pain. This can include asking for personal and family medical histories and of any recent injuries. Further diagnosis may include sensation tests, a physical examination, and potentially x-rays or other imaging tests.
Treatment
Just as the range of causes varies widely, so do treatments. Some more common treatments are rest, ice packs, keeping pressure off the foot, orthotics and braces, medication for inflammation and pain, and surgery.
If you have any questions, please feel free to contact our office located in Tipton, IN . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Various Causes of Ankle Pain
Ankles are joints that connect bones in the feet with bones in the lower leg. They are comprised of bones, ligaments, muscles, tendons, blood vessels, and nerves. The ankle joint allows the foot to move side-to-side, as well as up-and-down.
Ankle pain can be caused by a variety of conditions, but is most commonly due to soft tissue injuries such as ankle sprains and strains.
An ankle sprain occurs when one or more of the strong ligaments that support and stabilize the ankle become overly stretched or even torn if the ankle rolls, turns, or twists awkwardly. Depending on the grade of sprain (mild-moderate-severe), there will be varying degrees of pain, swelling, and restricted range of motion, along with tenderness, bruising, and ankle instability. There may even be an audible popping noise at the moment of injury.
Ankle strains can sometimes produce similar symptoms of pain, swelling, and loss of motion, however, they are due to overly stretched muscles and tendons—not ligaments. Ankle strains may also cause muscle cramps in the feet, calves and shins.
Ankle fractures are another common source of ankle pain and occur one or more of the three bones in the ankle become fractured (broken). These breaks can be stress fractures (due to repetitive stress) or traumatic fractures (due to an acute injury). Depending on where and how severe the fracture is, symptoms can include pain and swelling that can sometimes spread up to the knee, bruising or discoloration, and an inability to bear weight. A visible deformity or exposed bone may occur in severe fractures.
Various forms of arthritis may also cause ankle pain. Rheumatoid arthritis (RA) causes the immune system to attack healthy joints, like the ankle joint, by mistake, causing stiffness and swelling in both ankles. Osteoarthritis occurs when cartilage covering the ends of bones wears down, causing the bones to rub against each other. This results in pain, stiffness, and reduced range of motion in the ankle. Gout is a form of arthritis where excess amounts of uric acid in the bloodstream crystallize and build up on joints, causing severe pain and swelling. Reactive arthritis causes joint pain and swelling in the ankle in response to an infection in another part of the body.
Other forms of ankle pain include bursitis (an inflammation of a cushioning bursa sac between tendons and bone), scleroderma (a thickening of connective tissues), chronic ankle instability (caused by improperly healed ankle sprains), Achilles tendon injuries, flat feet, or an infection in the ankle.
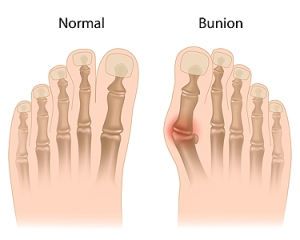
Managing Bunions
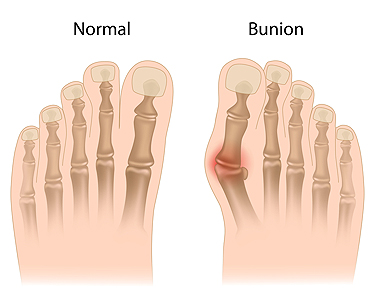
A bunion is a bony bump that forms at the base of the big toe, as the top of the toe angles toward the inner toes. This misalignment can lead to pain, swelling, and redness surroundig the joint. Over time, bunions may become more noticeable, with the bump growing larger and causing the skin to thicken or develop corns. Bunions are often caused by genetics, but factors like wearing tight shoes, high heels, or arthritis can also contribute. Symptoms include pain when walking, tenderness, and difficulty in finding comfortable shoes. Treatment options range from non-surgical to surgical solutions. A podiatrist can recommend changes to footwear, custom orthotics, and targeted exercises to ease pain and improve foot alignment. In more severe cases, surgery may be necessary to realign the toe and remove the bony bump. If you have a bunion causing discomfort or affecting your mobility, a podiatrist can provide personalized care. It is suggested that you schedule an appointment to explore your best treatment options.
If you are suffering from bunion pain, contact James Tyler Vestile, DPM of Foot and Ankle Centers of Indiana. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
Bunions are painful bony bumps that usually develop on the inside of the foot at the joint of the big toe. As the deformity increases over time, it may become painful to walk and wear shoes. Women are more likely to exacerbate existing bunions since they often wear tight, narrow shoes that shift their toes together. Bunion pain can be relieved by wearing wider shoes with enough room for the toes.
Causes
- Genetics – some people inherit feet that are more prone to bunion development
- Inflammatory Conditions - rheumatoid arthritis and polio may cause bunion development
Symptoms
- Redness and inflammation
- Pain and tenderness
- Callus or corns on the bump
- Restricted motion in the big toe
In order to diagnose your bunion, your podiatrist may ask about your medical history, symptoms, and general health. Your doctor might also order an x-ray to take a closer look at your feet. Nonsurgical treatment options include orthotics, padding, icing, changes in footwear, and medication. If nonsurgical treatments don’t alleviate your bunion pain, surgery may be necessary.
If you have any questions, please feel free to contact our office located in Tipton, IN . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Bunions
A bunion is a bump that forms at the base of the big toe. Bunions form when the big toe pushes against the next toe, which forces the big toe joint to get bigger and stick out. As a result, the skin over the bunion may start to appear red and it may feel sore.
There are risk factors that can increase your chances of developing bunions. People who wear high heels or ill-fitting shoes are more likely to develop them, in addition to those who have a genetic history of bunions or have rheumatoid arthritis.
The most obvious way to tell if you have a bunion is to look for the big toe pushing up against the toe next to it. Bunions produce a large protrusion at the base of the big toe and may or may not cause pain. Other symptoms are redness, swelling, and restricted movement of the big toe if you have arthritis.
Nonsurgical methods are frequently used to treat bunions that aren’t severe. Some methods of nonsurgical treatment are orthotics, icing and resting the foot, taping the foot, and pain medication. Surgery is usually only required in extreme cases. However, if surgery is needed, some procedures may involve removing the swollen tissue from around the big toe joint, straightening the big toe by removing part of the bone, or joining the bones of your affected joint permanently.
Your podiatrist will diagnose your bunion by doing a thorough examination of your foot. He or she may also conduct an x-ray to determine the cause of the bunion and its severity.
Relieving Foot Pain From Standing All Day

Standing for long hours at work can lead to foot pain, swelling, and fatigue. Over time, it may cause conditions like plantar fasciitis, Achilles tendonitis, bunions, or ankle instability. To prevent discomfort, wear supportive shoes with cushioning and arch support. Custom orthotics can help distribute pressure evenly. Taking short breaks to stretch and shift weight between feet can reduce strain. Standing on anti-fatigue mats provides extra cushioning, while compression socks help improve circulation and reduce swelling. Regular foot exercises, such as toe stretches and calf raises, can strengthen muscles and improve flexibility. Maintaining a healthy weight also reduces stress on the feet. If pain persists despite these efforts, it may indicate an underlying issue. If you have chronic pain, swelling, or numbness in your feet, it is suggested that you see a podiatrist for effective relief and treatment tips.
While working on the feet, it is important to take the proper care of them. For more information about working on your feet, contact James Tyler Vestile, DPM from Foot and Ankle Centers of Indiana. Our doctor will treat your foot and ankle needs.
Working on Your Feet
Standing on your feet for long periods of time can cause stress and pain in your feet. Your whole body may experience change in terms of posture, back pain, bunions, callouses and or plantar warts. There are ways to avoid these conditions with proper foot care, smart choices and correct posture.
Positive Changes
Negative heeled shoe – Choosing this shoe type places the heel slightly lower than the ball of the foot. These are great for overall foot health. Find shoes that fit you correctly.
Go barefoot – Our feet were not designed to be enclosed for all hours of the day. Try to periodically expose your feet to air.
Eliminate Pain
Foot Exercises – Performing simple exercises, incorporating yoga and doing stretches are beneficial. This will allow increased blood flow to the area and muscles of the foot.
Achilles tendon – Stretching the foot out flat on the floor will relax the calf muscles and tendon. These exercises can be performed almost anywhere. Make sure you add these exercises to your daily regimen.
With a little bit of this information and knowing more about foot health, you will notice changes. Foot stretches and proper footwear will help with pain and prevent further issues.
If you have any questions please feel free to contact our office located in Tipton, IN . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
How to Handle a Long Work Day on Your Feet
In 2014, the American Podiatric Medical Association surveyed 1,000 American adults and found that half of all respondents lived with foot pain. Fortunately, there are ways to avoid foot problems such as following a daily footcare routine and wearing proper footwear at work.
If you have a job that requires you to be on your feet, it is best that you do not wear flat sole shoes. Your heel should be slightly elevated (less than 2 inches, but at least ¼-inch) if you are going to be standing for a prolonged period. You should also make sure that the shoes you wear are not too small. Tight shoes may cut off circulation to your feet, which will result in pain and blisters. It is always best to purchase fitted shoes later in the day, because the feet tend to swell as the day progresses. It may also be helpful to buy shoes a half size larger if you plan on wearing custom orthotics or arch supports.
Your muscles may become stiff when you are constantly standing up. It is important to take breaks every hour to stretch and relax. One tip is to perform calf raises, because this exercise will help improve your circulation. To perform this stretch, you first need to stand on the edge of a step with your abdominal muscles pulled inward. You then need to grip the step with the balls of your feet with your heels hanging over the edge. Next, try to raise your heels above the step by a few inches while standing on your tiptoes; hold this pose for a second. You should then lower your heels back even to the platform. These calf raises should be done ten times for full effectiveness.
You should also take care of your feet while you are at home. One of the best ways to prepare your feet for a long day of work is to soak them in ice water. Doing so for 20 minutes will help fight the swelling and inflammation that results from being on your feet at work.
Nevertheless, if you are experiencing pain in your feet, you should seek help from your podiatrist. Your doctor will help treat any ailments you may have in addition to helping you prevent any other ailments from developing in the future.