
Managing an Ingrown Toenail

An ingrown toenail occurs when the edge of a toenail grows into the surrounding skin, causing pain, swelling, and redness. This condition commonly affects the big toe and can be caused by improper nail trimming, wearing tight shoes, or injury. People with naturally curved nails or certain foot conditions are more prone to developing ingrown toenails. Symptoms include sharp pain, swelling, redness, and in some cases, the formation of pus if an infection develops. The area surrounding the nail may feel tender or sore, especially when walking or wearing shoes. Treatment for an ingrown toenail starts with soaking the foot in warm water to reduce swelling. For mild cases, a podiatrist may lift the nail or trim it carefully. In more severe cases, part of the nail may need to be removed or treated with a local anesthetic. If you are experiencing an ingrown toenail, it is suggested that you schedule an appointment with a podiatrist for proper care.
Ingrown toenails may initially present themselves as a minor discomfort, but they may progress into an infection in the skin without proper treatment. For more information about ingrown toenails, contact James Tyler Vestile, DPM of Foot and Ankle Centers of Indiana. Our doctor can provide the care you need to keep you pain-free and on your feet.
Ingrown Toenails
Ingrown toenails are caused when the corner or side of a toenail grows into the soft flesh surrounding it. They often result in redness, swelling, pain, and in some cases, infection. This condition typically affects the big toe and may recur if it is not treated properly.
Causes
- Improper toenail trimming
- Genetics
- Improper shoe fitting
- Injury from pedicures or nail picking
- Abnormal gait
- Poor hygiene
You are more likely to develop an ingrown toenail if you are obese, have diabetes, arthritis, or have any fungal infection in your nails. Additionally, people who have foot or toe deformities are at a higher risk of developing an ingrown toenail.
Symptoms
Some symptoms of ingrown toenails are redness, swelling, and pain. In rare cases, there may be a yellowish drainage coming from the nail.
Treatment
Ignoring an ingrown toenail can have serious complications. Infections of the nail border can progress to a deeper soft-tissue infection, which can then turn into a bone infection. You should always speak with your podiatrist if you suspect you have an ingrown toenail, especially if you have diabetes or poor circulation.
If you have any questions, please feel free to contact our office located in Tipton, IN . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Ingrown Toenails
Ingrown toenails (onychocryptosis) are a common foot ailment and it is very unpleasant to experience. The condition is caused by an increase in pressure from the ingrowth of the nail edge into the skin of the toe. Ingrown toenails commonly cause pain in those who experience them. In some cases, the skin surrounding the ingrown toenail may break which may lead bacteria to enter through and cause an infection. Common symptoms of this ailment include pain, redness, swelling, and warmth around the toe.
An imbalance between the size of the nail and the enlargement of the nail skin edge causes ingrown toenails. This condition is often caused by improperly trimming the toenails. If you are trying you cut your nails, you should always try to trim straight across instead of in a rounded shape. Ingrown toenails can also be an inherited condition and they may also be caused by improper shoe fitting.
Another common cause of the condition is wearing shoes that are either too small or too large. Other causes include poor foot hygiene, obesity, diabetes, arthritis, edema, and fungal infections. There are many risk factors that may make a person more likely to develop an ingrown toenail. Athletes who play “stop and start” sports such as tennis, soccer, and basketball are most likely to have ingrown toenails.
People who have diabetes, a compromised immune system, or poor circulation should immediately seek care from a podiatrist if they have an ingrown toenail. It is also recommended to seek professional assistance if at-home remedies are not successful within a week or if there is persistent pain.
Treating Diabetic Foot Ulcers

Diabetic foot ulcers are open wounds that develop due to skin breakdown, often caused by pressure, friction, or injury. People with diabetes are particularly at risk of foot ulcers because conditions like peripheral neuropathy and poor circulation can impair sensation and healing in the feet. Diabetic foot ulcers can appear on the toes, soles, or ankles and may progress to deeper layers, involving muscles, tendons, or even bones. Untreated foot ulcers increase the risk of infection, potentially leading to severe complications, like gangrene or limb loss. A podiatrist plays a key role in managing diabetic foot ulcers by performing wound care, including debridement to remove damaged tissue and applying specialized dressings to promote healing. They may also recommend offloading techniques, such as using custom footwear or casts to reduce pressure on the affected area. Regular monitoring is essential to catch any early signs of infection or worsening ulcers. If you have foot ulcers related to diabetes, it is suggested that you make an appointment with a podiatrist for regular exams and necessary treatment.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with James Tyler Vestile, DPM from Foot and Ankle Centers of Indiana. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in Tipton, IN . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
Arthritis Can Cause Pain in the Feet and Ankles
Mistakes to Watch for in Treating Toenail Fungus
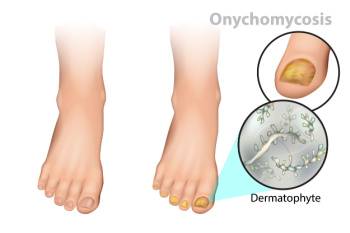
Toenail fungus, or onychomycosis, is a common infection that can cause thickened, discolored, and brittle nails. Mistakes in managing it often worsen the condition. Ignoring early signs like slight discoloration or nail brittleness can allow the infection to spread. Mild treatments might help, but using them inconsistently or stopping too soon often leads to recurrence. Another mistake is attempting to self-treat with home remedies without proper diagnosis, delaying effective care. Wearing tight, non-breathable shoes or walking barefoot in public areas like pools or gyms increases reinfection risks. Poor nail hygiene, such as improper nail trimming or sharing nail tools also contributes to fungal growth. Treating toenail fungus requires patience and consistency. If you have this condition, it is strongly suggested that you see a podiatrist for effective and safe treatment.
If left untreated, toenail fungus may spread to other toenails, skin, or even fingernails. If you suspect you have toenail fungus it is important to seek treatment right away. For more information about treatment, contact James Tyler Vestile, DPM of Foot and Ankle Centers of Indiana. Our doctor can provide the care you need to keep you pain-free and on your feet.
Symptoms
- Warped or oddly shaped nails
- Yellowish nails
- Loose/separated nail
- Buildup of bits and pieces of nail fragments under the nail
- Brittle, broken, thickened nail
Treatment
If self-care strategies and over-the-counter medications does not help your fungus, your podiatrist may give you a prescription drug instead. Even if you find relief from your toenail fungus symptoms, you may experience a repeat infection in the future.
Prevention
In order to prevent getting toenail fungus in the future, you should always make sure to wash your feet with soap and water. After washing, it is important to dry your feet thoroughly especially in between the toes. When trimming your toenails, be sure to trim straight across instead of in a rounded shape. It is crucial not to cover up discolored nails with nail polish because that will prevent your nail from being able to “breathe”.
In some cases, surgical procedure may be needed to remove the toenail fungus. Consult with your podiatrist about the best treatment options for your case of toenail fungus.
If you have any questions, please feel free to contact our office located in Tipton, IN . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Treating Toenail Fungus
Fungal infection of the toenail, or onychomycosis, typically appears as a gradual change in a toenail’s texture and color that involves brittleness and darkening. The fungal infection itself occurs beneath the surface of the nail. Aside from discoloration, other symptoms include the collection of debris beneath the nail plate, white marks on the nail plate, and a foul odor emanating from the nail. If ignored, the infection can spread into other nails and the skin; in severe cases, it can hinder one’s ability to work or walk.
The toenails are particularly vulnerable to contracting infection in moist environments where people are likely to be walking barefoot, such as around swimming pools, public showers, and locker rooms. Fungal infection may also be more likely to occur in nail beds that have been injured, and sufferers of chronic diseases such as diabetes, circulatory problems, or immunodeficiency conditions are particularly prone to developing fungal nails.
Fungal nails can be primarily prevented by practicing proper hygiene and regularly examining the feet and toes. Carefully washing the feet with soap and water and thoroughly drying the feet afterwards are essential. Other tips include wearing shower shoes in public areas, changing shoes and socks daily, keeping toenails clipped at a short length, wearing breathable shoes that fit properly, wearing moisture-wicking socks, and disinfecting home pedicure tools and instruments used to cut nails.
Fungal nail treatment may vary between patients and the severity of the condition. Your podiatrist may suggest a daily routine of cleansing that spans over a period of time to ease mild infections. Over-the-counter or prescription antifungal agents may also be prescribed, including topical and/or oral medications. Debridement, or the removal of diseased nail matter and debris, may also be performed. In more severe cases, surgical treatment may be needed. In some instances, the temporary removal of the fungal nail allows for the direct application of a topical antifungal to the nail bed. In other cases, a chronically painful fungal nail that has not responded to other treatments may be permanently removed; this allows the infection to be cured and avoids the growth of a deformed nail.
Reasons for Pins and Needles in the Feet

Pins and needles in the feet, medically known as paresthesia, can arise from a variety of causes that often involve the nerves in the feet, toes, or ankles. Diabetes and alcohol abuse frequently lead to peripheral neuropathy, where prolonged high blood sugar levels damage the nerves, resulting in tingling or numbness. Tarsal tunnel syndrome, caused by compression of the tibial nerve in the ankle, is another possible cause of burning and tingling pain. Vitamin deficiencies, particularly B12, may also contribute to nerve dysfunction, resulting in tingling sensations. Inherited conditions like Charcot-Marie-Tooth disease can weaken the peripheral nerves and cause persistent tingling and numbness. Exposure to certain toxins or medications can similarly affect nerve health. A podiatrist can evaluate your symptoms through a physical exam, diagnostic tests, and a review of your medical history to determine the underlying cause. If you frequently experience a feeling of pins and needles in your feet, it is suggested that you schedule an appointment with a podiatrist for a thorough exam.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with James Tyler Vestile, DPM from Foot and Ankle Centers of Indiana. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our office located in Tipton, IN . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Foot Pain
Our feet are arguably the most important parts of our bodies because they are responsible for getting us from place to place. However, we often don’t think about our feet until they begin to hurt. If you have pain in your feet, you need to first determine where on the foot you are experiencing it to get to the root of the problem. The most common areas to feel pain on the foot are the heel and the ankle.
Heel pain is most commonly attributed to a condition called plantar fasciitis. Plantar fasciitis occurs when the plantar fascia, which is the band of tough tissue connecting the heel bone to the toes becomes inflamed. Plantar fasciitis pain is usually worse in the morning, and it tends to go away throughout the day. If you have plantar fasciitis, you should rest your foot and do heel and foot muscles stretches. Wearing shoes with proper arch support and a cushioned sole has also been proven to be beneficial.
Some common symptoms of foot pain are redness, swelling, and stiffness. Foot pain can be dull or sharp depending on its underlying cause. Toe pain can also occur, and it is usually caused by gout, bunions, hammertoes, ingrown toenails, sprains, fractures, and corns.
If you have severe pain in your feet, you should immediately seek assistance from your podiatrist for treatment. Depending on the cause of your pain, your podiatrist may give you a variety of treatment options.
Symptoms and Diagnosis of Flat Feet

Flat feet, also known as fallen arches, is a condition where the arch of the foot collapses or does not form properly. This leads to the entire sole of the foot making contact with the ground. The most common symptoms of flat feet include foot pain, particularly in the arch or heel area, swelling along the inner part of the foot, and difficulty standing or walking for extended periods. People with flat feet may also experience problems with balance and a tendency to tire quickly. Diagnosing flat feet typically involves a physical examination by a podiatrist, who will look for visible signs of the condition. X-rays or other imaging tests may be used to assess the alignment of the bones in the foot. If you have flat feet that are causing pain and discomfort, it is suggested that you consult a podiatrist who can offer you effective relief and treatment solutions.
Flatfoot is a condition many people suffer from. If you have flat feet, contact James Tyler Vestile, DPM from Foot and Ankle Centers of Indiana. Our doctor will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
- Pain around the heel or arch area
- Trouble standing on the tip toe
- Swelling around the inside of the ankle
- Flat look to one or both feet
- Having your shoes feel uneven when worn
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions please feel free to contact our office located in Tipton, IN . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.







